Diabetes Type 2 Obesity Prediabetes Weight Loss Diabetes Metabolic Appetite
Obesity Prediabetes Diabetes Recovery Protocols
Diabetes Protocol
CORE PROTOCOLS >>
Diabeta Lean
Forskolin one capsule twice per day
Biotin Plus one to two capsules before meals
DiabetaLean two caps before meals
GlycemX Meal replace one meal plus per day
Chromium Organic one capsule twice per day
Power C PLUS three capsules twice per day
NutrImmune 26Y one capsule twice per day
Power Methyl B12 one capsule sublingual twice per day
VitaMineralMAX one capsule twice per day with
Minerals Plus one capsule twice per day
NutrioDine 10 drops in filtered water twice per day
MicroDose HGH three to four sprays sublinqually four times peer day
Indium-Me 5 drops AM and bedtimes sublinqually
Royal Jelly two softgels twice per day
Low Glycemic 25, Low Lectin, No Gluten Diet
Meals only 11 AM to 7 PM, Fast Rest of Day with Fluids No Sugar, or Sweetners Artificial Asparatame Splenda, etc.
Advanced:
Carnosine D-Link one to two capsules twice per day
NutriTRALA one tablet twice per day
MitoThyroid two capsule in AM and repeat if Oral temp is less by one half degrees Celcius at lunch times
CoQ10 Supreme Ubiquinol two softgels twice per day
Pancreatic and Vacular Peptides twice per day month one, then once per day before supper meals
SonicLIFE machine exercise therapy with Mineral Resonance Fields and Nagalase Frequencies Plus future organ specific tripeptide frequencies
Red Deer Velvet DR three to four capsules twice per day
MyCell D3 5,000 IU two softgels twice per day
Lumen Photon over pancreas Setting 4 and over muscles and liver Setting 3 for 15 to 30 minutes two to three times per day

We should all be familiar with the idea that food intake is energy intake. And when one eats too much, they are taking in too much energy – and if this energy is not used in active processes in the body, it will be stored. Most of it will be stored as fat. Obese states occur when energy intake chronically exceeds energy expenditure, as all the excess energy is locked up in the extensive fat reserves.  The specialized cells which store fat are called adipocytes, and fatty tissue is referred to as adipose. An interesting observation is that an adult who becomes obese has the same number of adipocytes as they did when they were lean. The idea being that at around the age of 8 or so, one stops producing any significant number of adipocytes. Past this, more fat is packed into the existing cells, so they just swell up. It seems that some people may be primed to put on more weight because of a greater existing number of adipocytes produced during childhood, because they have more ‘storage space’ in which to pack fat.
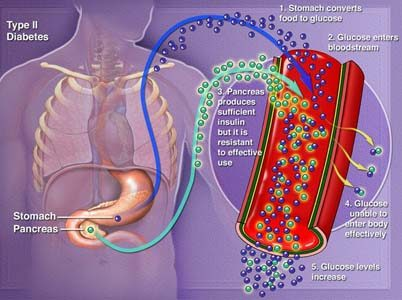
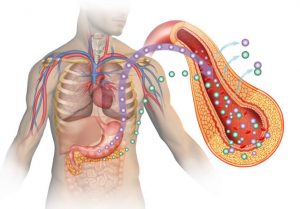
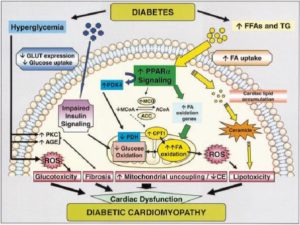
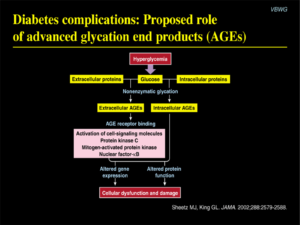
The specialized cells which store fat are called adipocytes, and fatty tissue is referred to as adipose. An interesting observation is that an adult who becomes obese has the same number of adipocytes as they did when they were lean. The idea being that at around the age of 8 or so, one stops producing any significant number of adipocytes. Past this, more fat is packed into the existing cells, so they just swell up. It seems that some people may be primed to put on more weight because of a greater existing number of adipocytes produced during childhood, because they have more ‘storage space’ in which to pack fat.  light micrograph of adipose tissueAdipose tissue is more than just a fatty store, though. It is also an active endocrine organ, releasing chemical signals into the bloodstream to signal to the brain and the rest of the body about its current energy state, so the body can adjust its function and behaviour to meet its current needs. Obesity is more than simply being overweight, however. There are major imbalances that occur within the body prior to, and as a result which make this such an important disease in the modern world. During obesity, tissues become desensitised to chemical signals which would usually signal to them to decrease food intake, or to increase energy expenditure. Examples of this are the decreased effect of leptin in the feeding-control-centres of the hypothalamus, leptin on skeletal muscle and adiponectin on the brain and skeletal muscle. These are signals which would ordinarily decrease energy intake by modifying behaviour and metabolism, thus keeping weight down. But in obesity, they become dysregulated. As a result, cells become more prone to store energy as fat, and feeding centres in the brain become impaired. Furthermore, obesity is linked to type II diabetes. The excess expansion of adipocytes from all their fat uptake can stimulate inflammatory immune cells (via hypoxia-induced mechanisms) which can damage the insulin secreting cells of the pancreas. The excess fatty acids present in circulation can also act to inhibit the glucose sensing mechanisms in these insulin secreting cells. This leads to dysregulation of glucose homeostasis, and what we consider to be Diabetes mellitus, aka Type II Diabetes.
light micrograph of adipose tissueAdipose tissue is more than just a fatty store, though. It is also an active endocrine organ, releasing chemical signals into the bloodstream to signal to the brain and the rest of the body about its current energy state, so the body can adjust its function and behaviour to meet its current needs. Obesity is more than simply being overweight, however. There are major imbalances that occur within the body prior to, and as a result which make this such an important disease in the modern world. During obesity, tissues become desensitised to chemical signals which would usually signal to them to decrease food intake, or to increase energy expenditure. Examples of this are the decreased effect of leptin in the feeding-control-centres of the hypothalamus, leptin on skeletal muscle and adiponectin on the brain and skeletal muscle. These are signals which would ordinarily decrease energy intake by modifying behaviour and metabolism, thus keeping weight down. But in obesity, they become dysregulated. As a result, cells become more prone to store energy as fat, and feeding centres in the brain become impaired. Furthermore, obesity is linked to type II diabetes. The excess expansion of adipocytes from all their fat uptake can stimulate inflammatory immune cells (via hypoxia-induced mechanisms) which can damage the insulin secreting cells of the pancreas. The excess fatty acids present in circulation can also act to inhibit the glucose sensing mechanisms in these insulin secreting cells. This leads to dysregulation of glucose homeostasis, and what we consider to be Diabetes mellitus, aka Type II Diabetes.  Adipose as an endocrine organ, and some of its roles in hormonal signalling The underlying biochemistry of obesity shows that there may be certain genetic predispositions which make it more likely for somebody to enter an obese state. Some may shrug this aside as saying ‘You’re just giving fat people an excuse’. But that isn’t the point. Such sentiments merely reflect the negative social stigma attached to obesity, which leads to the psychological impact of obesity on the patient. These social pressures make obesity more than just a disorder of energy regulation, but a disorder which affects psychological state. Predispositions may occur via polymorphism of the structure of hormone-responsive receptors which mediate energy regulating behaviour or metabolism, through variation in horomone secretion patterns, the number of adipocytes one has, amongst many others. Likewise, it’s progression into diabetes relies on multiple imbalances and factors which just complicate the whole diabetes/obesity picture somewhat.
Adipose as an endocrine organ, and some of its roles in hormonal signalling The underlying biochemistry of obesity shows that there may be certain genetic predispositions which make it more likely for somebody to enter an obese state. Some may shrug this aside as saying ‘You’re just giving fat people an excuse’. But that isn’t the point. Such sentiments merely reflect the negative social stigma attached to obesity, which leads to the psychological impact of obesity on the patient. These social pressures make obesity more than just a disorder of energy regulation, but a disorder which affects psychological state. Predispositions may occur via polymorphism of the structure of hormone-responsive receptors which mediate energy regulating behaviour or metabolism, through variation in horomone secretion patterns, the number of adipocytes one has, amongst many others. Likewise, it’s progression into diabetes relies on multiple imbalances and factors which just complicate the whole diabetes/obesity picture somewhat.
Figure 1. The effects of ghrelin on the CNS, and subsequent glucose, lipid and energy metabolism.
(A) Ghrelin is secreted mainly by the stomach, and can (B) have paracrine or endocrine effects on GI motility or (C) circulate in the blood and act on CNS growth hormone secretagogue receptors (GHS-Rs) inside and outside the blood–brain barrier. Known target areas in the CNS include the hypothalamus, the ventral tegmentum and nucleus accumbens, the hippocampus and GHS-R populations in the brainstem area. The actions of ghrelin in the CNS contribute (D) to the control of food intake and (E) co-regulate tissue-specific cellular pathways in the periphery, thereby governing glucose, lipid and energy metabolism. Control of peripheral metabolism by ghrelin and the CNS is mediated by the autonomic nervous system as well as the hypothalamic–pituitary endocrine axes. Apart from in the stomach, ghrelin is produced in a variety of peripheral tissues, although to a very low extent. (F) Paracrine ghrelin secretion from pancreatic cells might, however, be of importance for the inhibition of insulin secretion from  cells as well as for
cells as well as for  -cell viability. Abbreviations: BAT, brown adipose tissue; CNS, central nervous system; GI, gastrointestinal; WAT, white adipose tissue.
-cell viability. Abbreviations: BAT, brown adipose tissue; CNS, central nervous system; GI, gastrointestinal; WAT, white adipose tissue.
Disclaimer: These Wellness Protocols are not intended to replace the attention or advice of a physician or other qualified healthcare professional. These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease.